eliability evaluation of alumina-blasted/acid-etched versus laser-sintered dental implants
Step-stress accelerated life testing (SSALT) andfractographic analysis were performed to evaluate the reli-ability and failure modes of dental implant fabricated bymachining (surface treated with alumina blasting/acid etch-ing) or laser sintering for anterior single-unit replacements.Forty-two dental implants (3.75×10 mm) were divided intwo groups (n021 each): laser sintered (LS) and aluminablasting/acid etching (AB/AE). The abutments werescrewed to the implants and standardized maxillary centralincisor metallic crowns were cemented and subjected toSSALT in water. Use-level probability Weibull curves andreliability for a mission of 50,000 cycles at 200 N werecalculated. Polarized light and scanning electron micro-scopes were used for failure analyses. The Beta (β) valuederived from use-level probability Weibull calculation of1.48 for group AB/AE indicated that damage accumulationlikely was an accelerating factor, whereas theβof 0.78 forgroup LS indicated that load alone likely dictated the failuremechanism for this group, and that fatigue damage did notappear to accumulate. The reliability was not significantlydifferent (p>0.9) between AB/AE (61 %) and LS (62 %).Fracture of the abutment and fixation screw was the chieffailure mode. No implant fractures were observed. No dif-ferences in reliability and fracture mode were observedbetween LS and AB/AE implants used for anterior single-unit crowns.
KeywordsDental implant.Reliability.Laser solid-state.Step-stress accelerated life testing.
dental laser tips
Introduction
It is general consensus that rough implant surfaces are moreosteoconductive than smooth surfaces, [1–3] and result inhigh long-term survival and success rates [4–6]. Surfacetexturing is commonly employed as one of the final stepsprior to cleaning, packaging, and sterilizing dental implants,and such procedures may have drawbacks such as increasedfinal cost and potential implant contamination with blastingmedia and organic contaminants from surface processingwhich may jeopardize osseointegration [7]. Thus, alternativemethods which allow surface texturing during the manufac-turing process are desirable.
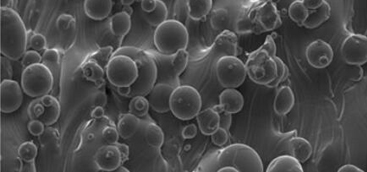
The laser metal-sintering process is a technology thatproduces solid metal components with intricate porous ge-ometries [1,2]. Potential advantages of laser sintering ishigh throughput manufacturing along with potential im-proved properties such as the elastic properties that may betailored to more closely match those of bone [2,8], poten-tially improving the bone–implant complex biomechanics [9,10]. Advantages also include that implants may bemanufactured from commercially pure titanium or alloys [8].From a host response to laser-sintered implants perspec-tive, a previous study have demonstrated acceptableosseointegration levels to laser-modified implants relativeto alumina-blasted/acid-etched implants, along with differ-ent fracture patterns between the interface and bone follow-ing mechanical testing [11,12]. Transmission electronmicroscopy and chemical analysis showed coalescence be-tween mineralized tissue and the surface of the laser-modified implant [13]. Recently, improved biomechanicalresponse has been reported for laser-sintered compared toalumina-blasted/acid-etched implants at early times (1 and6 weeks in vivo) [14]. A human retrieval study [8] showedthat the laser-sintered surface presented a close contact withthe bone after 8 months in vivo. However, it is unclear if thelaser sintering alters the mechanical behavior of the implant.While the biocompatibility of implants fabricated by thelaser-sintering process has been demonstrated [1], limita-tions that are inherent to sintering processes such as thepotential for flaws in the material surface and bulk has raisedconcerns when it comes to their mechanical performance.
Conclusion
The postulated hypothesis that different implant fabricationmethods result in different reliability and failure modeswhen subjected to step-stress accelerated life testing wasrejected. When varying the implant fabrication method, nosignificant differences were observed in values of reliabilityafter SSALT.