Abstract
Background
Periodontitis is an inflammatory disease of the supportive tissue of teeth caused by specific microorganisms. Periodontitis is a typical example of a chronic inflammatory reaction which cannot develop without an associated inflammation, since it is always attended by gingivitis with marked inflammation. The aim of the paper is to show the anti-inflammatory effects on gingiva by combined therapy (conservative therapy complemented with laser therapy).
Material and methods
A total of 34 patients were examined who had been diagnosed with chronic periodontitis. In the experimental group 17 patients were treated using conservative methods (scaling and root planing) followed by a low level laser therapy (LLLT) with a Scorpion-SM-405-7A system (OPTIKA-LASER; Sofia, Bulgaria), and the patients of the control group (n = 17) were treated only with scaling and root planing (SRP).
Clinical measurements included probing pocket depth (PPD), bleeding on probing (BOP), clinical attachment level (CAL), as well as supragingival plaque measurements (PL) and gingival crevicular fluid (GCF) measurements in pockets and were undertaken before therapy (baseline), and three and six months, respectively after the therapy had been completed.
Results
All the subjects in each group completed all phases of the study. Six months after the therapy, the average PPD, CAL and CGF reduction in the experimental group with LLLT was significantly greater (p < 0.05) than for the patients receiving only conservative therapy. The reduction in CAL and GCF at the treated sites was greater than at the SRP sites, although the difference was statistically significant for the six month visit only (p < 0.05).
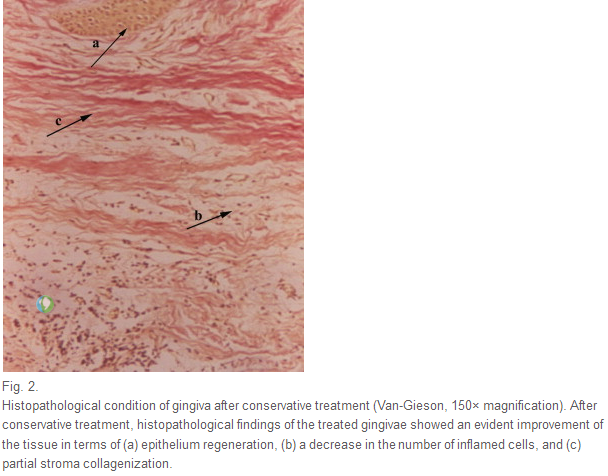
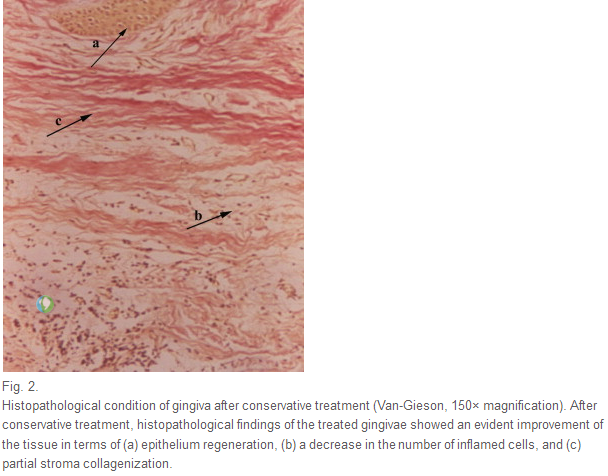
In the group using only conservative therapy, histological findings of gingivae showed a reduction in the number of inflammatory cells and partial stroma collagenization, while histological findings in gingivae after the laser therapy indicated completely regenerated gingival tissue with few inflammatory cells as well as marked collagen tissue homogenization.
Conclusion
Based on the results obtained, it can be concluded that the use of LLLT as an adjunct procedure in the conservative treatment of periodontitis is very successful in reducing gingival tissue inflammation.
Hintergrund
Parodontitis ist eine entzündliche Erkrankung des Zahnhalteapparates hervorgerufen durch Bakterien. Eine Parodontitis (Zahnbettentzündung) geht immer mit einer Gingivitis (Zahnfleischentzündung) einher. Ziel der vorgelegten Studie war es daher, die antientzündlichen Effekte einer kombinierten Therapie (konventionelle Therapie mit anschließender Softlasertherapie) auf die Gingiva zu untersuchen.
Material und Methoden
Insgesamt wurden 34 Patienten mit diagnostisch gesicherter chronischer Parodontitis in die Studie eingeschlossen. Die Hälfte der Patienten (n = 17) wurde zunächst konservativ mittels Kürettage behandelt, gefolgt von einer Low-Level-Lasertherapie (Scorpion-SM-405-7A; OPTIKA-LASER, Sofia, Bulgarien). Die andere Hälfte der Patienten wurde nur konservativ behandelt (Kontrollgruppe).
Die klinische Evaluation erfolgte jeweils vor sowie 3 und 6 Monate nach Behandlung durch Messung der Sondierungstiefen (probing pocket depth, (PPD)) und des Attachmentlevels (clinical attachment level, (CAL)) sowie durch Beurteilung der Sondierungsblutung (bleeding on probing, (BOP)). Es wurde außerdem eine Plaquekontrolle durchgeführt sowie der Sulkusfluid (gingival crevicular fluid, (GCF)) in den Zahnfleischtaschen gemessen.
Ergebnisse
Alle Patienten durchliefen die Studie vollständig. 6 Monate nach Therapie waren in der Gruppe, die sich einer kombinierten Therapie mit Low-Level-Laserbehandlung unterzogen hatte, die mittleren Sondierungstiefen, Attachmentlevel und Sulkusfluidmengen gegenüber der Kontrollgruppe mit ausschließlich konservativer Behandlung signifikant reduziert (p < 0.05).
Vergleicht man die absoluten Werte für CAL und GCF miteinander, so war die Reduktion in der kombinierten Behandlungsgruppe (ΔCAL = 0.97 mm, ΔGCF = 0.0022 ml) größer als in der Kontrollgruppe (ΔCAL = 0.64 mm, ΔGCF = 0.002 ml), auch wenn diese Differenzen nur für die 6-Monats-Kontrolluntersuchung statistisch signifikant waren (p < 0.05).
Die histologischen Untersuchungen der Gingiva ergaben in der Kontrollgruppe einen Rückgang der Entzündungszellen und eine partielle Stromakollagenisierung. In der kombinierten Behandlungsgruppe zeigte sich eine komplette Regeneration der Gingiva mit nur noch wenigen Entzündungszellen und homogenem Bindegewebe.
Zusammenfassung
Die Ergebnisse der vorgelegten Studie zeigen, dass in der konservativen Parodontitisbehandlung eine ergänzende Behandlung mit dem Softlaser entzündungshemmende Wirkung auf die Gingiva hat.
Schlüsselwörter
Parodontitis; Softlaser; Klinische Parameter; Histopathologie
Keywords
Periodontitis; Low level laser; Clinical parameters; Histopathology;
dental laser tips
Introduction
Chronic periodontitis is an inflammatory disease that results in the destruction of the soft tissue and supporting bone structure of the periodontium (periodontal membrane and alveolar bone), with the formation of periodontal pockets and gingival recession [1].
Certain Gram-negative bacteria have been implicated in the pathogenesis of this disease including Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans and Tannerella forsythensis [2]. These microorganisms, found in the gingival sulcus, are responsible for the first pathological changes in the inflamed gingiva. The first damage is the widening of the intracellular spaces, which during the early phase of gingival inflammation enables aggressive bacteria and their products to penetrate into the connective gingival tissue [3].
The disease starts with gingival inflammation which develops through several phases to the point that it affects other parts of periodontium, and finally results in periodontitis. The changes, taking place at the blood vessels level, appear as the first manifestations of gingival inflammation (‘initial lesion’). The capillaries dilate and there is an increase in the blood flow [4]. In the ‘early lesion’, the changes noted in the ‘initial lesion’ become more marked, the volume of inflammatory infiltrate also increases which clinically results in gingival enlargement [5]. A ‘developed lesion’ occurs as a consequence of dental plaque persistence when some of the bacteria may penetrate into the host tissue. Perivascular accumulation of chronic inflammatory cells is evident at this stage [6]. However, there is still no loss of the bone or connective tissue attachment. Chronic periodontitis is characterized by the loss of the connective tissue attachment and alveolar bone. Clinically, the process is manifested as formation of a periodontal pocket [2].
Periodontitis manifests itself as a disease which cannot develop without the associated inflammation because it is always preceded by gingivitis with marked inflammation.
Only a decade ago laser therapy was thought to be an absolute novelty in Serbian dentistry, a little bit futuristic, promising but still controversial. Today it is a standard dentistry procedure with clearly defined indications and contraindications and has lost the label of an experimental medical procedure.
A laser is considered to be basically effective for treating periodontal diseases because of its excellent physical properties, namely ablation, hemostasis, killing of bacteria and cell stimulation. The low level laser light has wide range of proved therapeutic possibilities in oral medicine and periodontology. Nakova et al. [7] noted a significant reduction of gingival inflammation, which is the result of anti-inflammatory, anti-edematous laser activity, as well as intensification of humoral and cellular immunity and acceleration of reparatory and regeneratory capabilities.
This therapeutic laser treatment, also referred to as low level laser therapy (LLLT), offers numerous benefits. Along with the primary benefit of being non-surgical, it promotes tissue healing and reduces edema, inflammation, and pain [8]; [9] ; [10].
Dental laser therapy has been in use for over 30 years and more than 90% of the available literature reports positive effects [11]; [12] ; [13]. Sometimes it is used as a part of a therapy, and sometimes it is used as monotherapy [14] ; [15].
The aim of the study was to evaluate the efficacy of LLLT combined with conservative therapy in the treatment of periodontitis patients and to analyze the clinical results and histopathological findings as well as to confirm its use as an adjunct to scaling and root planing (SRP).
Material and methods
Patient population
Thirty-four patients, 20 males and 14 females, with an average age of 45 years were randomly selected to take part in the study. One criterion for inclusion in the study was that all patients were scheduled for the extraction of at least one tooth because of prosthetic and/or orthodontic reasons. All the patients were registered at the Department of Periodontology and Oral Medicine of the Clinic of Dentistry in Nis. They all gave their written consent to be included in the study. The protocol of investigation was approved by the Scientific Ethical Committee of Medical Faculty in Nis (No: 01-2800-5).
All the patients suffered from chronic periodontitis with marked clinical symptoms of gingival inflammation. The diagnosis of periodontitis was made on the basis of classic diagnostic methods: anamnesis, clinical presentation, an index of gingival oral hygiene, and radiographs.
Persons excluded from the research were those suffering from any systemic disease, smokers, pregnant women, subjects currently under periodontal therapy, subjects taking antiobiotics or those who had taken antibiotics six months prior to the research. A split-mouth design was not considered for the investigation.
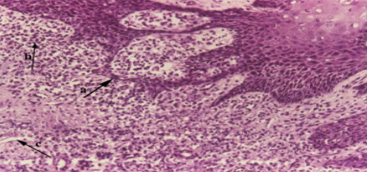
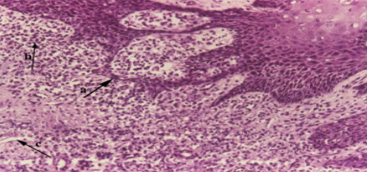
Fig. 1.
Histological findings (HE, 150× magnification) of the inflamed gingiva before treatment showed: (a) a thickening of the basal layer of gingival epithelium with partial damage, (b) a marked inflammation in the connective tissue, and (c) numerous blood vessels.
The group was divided into two groups of 17 patients each. The first group of patients was the experimental (E) group given combined therapy (conservative complemented with laser therapy), which means that conservative treatment (SRP) preceded the LLLT. The second group, the control (C) group, was made up of 17 patients who were only treated with conservative methods (SRP). They were treated following the same principles and schedule as the experimental group, but without additional application of the low level laser.
Clinical measurements were carried out before therapy (baseline), as well as three and six months after the therapy had been completed.
Clinical measurements
Clinical response was assessed by measuring periodontal probing depth (PPD) (from free gingival margin to the bottom of the periodontal pocket), clinical attachment level (CAL) (from enamel cement margin to periodontal pocket), and plaque score (PI) based on a modified score of 0–3. The PIs were recorded as follows: ‘0’ = no plaque present; ‘1’ = plaque covering not more than one third of the tooth; ‘2’ = plaque covering more than one third but not more than two thirds of the exposed tooth surface; ‘3’ = plaque covering more than two thirds of the exposed tooth surface. Moreover, bleeding on probing (BOP) was evaluated using a scoring scheme, where ‘0’ = no bleeding; ‘1’ = bleeding within 10 s after probing; ‘2’ = bleeding within probing, ‘3’ = spontaneous bleeding. The plaque index was measured by applying organic colors on teeth (gentian violet) and using sterile dental mirrors and explorers to assess plaque accumulation and gingival status. PPD, CAL and BOP were measured using a standardized Michigan O periodontal probe. Samples of gingival crevicular fluid (GCF) were obtained using a paper filter strip following a 10 s sample into the periodontal pocket depth.
Low level laser therapy
After the conservative therapy, which comprised 10 treatment sessions, the patients in the experimental group were treated using the low level laser according to the following procedure and parameters.
The laser used in the study was a Scorpion-SM-405-7A system (OPTIKA-LASER; Sofia, Bulgaria), which is a semi-conductive laser for oral application operating at a wavelength of 670 nm. Laser radiation was applied via an optical fiber with a spot width of 3 mm, a power density of 150 mW/cm2, an energy density of 4 J/cm2, and a power output of 10 mW. Laser irradiation was conducted every day after conservative instrumental treatment of the periodontal pockets for 10 days. The tip was set to continuous mode and applied and kept in light contact for 15 s with the gingival tissues around every tooth (facial and lingual) for approximately 4 min per quadrant. The laser beam was directed at an angle of 90° in relation to gingival surface, with the laser tip 2 mm from the surface.
Histopathological evaluation
Gingiva of all patients were examined histologically at the baseline (before therapy) and after the therapy (either only conservative therapy or combined therapy). The gingival biopsy was taken from the teeth that had been previously marked for extraction, for prosthetic and orthodontic reasons. Histopathological examinations were carried out at the Institute of Pathology of the Faculty of Medicine in Nis.
For the tissue samples the following staining methods were applied:
• Hematoxylin–Eosin (HE) for verification of histopathological processes.
• Van-Gieson's histochemical method for collagen fiber staining.
Statistical analysis
Statistical analysis was performed by descriptive and analytic statistic methodology using standard data processing programs MS Excel and SPSS program package, version 10.0. The following statistical parameters were displayed: arithmetic mean, standard deviation (SD). Testing was done by χ2-test, t-test and Pearson's chi-square test (significance level: α = 0.05).
Results
Comparison of clinical parameters
Mean clinical scores in clinical measurements demonstrated that no significant differences among the both groups (E and C) were noted for PPD (p > 0.05), CAL (p > 0.05), BOP (p > 0.05), and PI (p > 0.05), on the baseline measurement but a difference was found for GCF (p = 0.0001)
Discussion
Periodontal disease belongs to the class of inflammatory conditions of the supportive tissue of teeth which are caused by bacteria. In recent years scientists have found increasingly more facts to support the theory that gingival inflammation, besides the age and presence of deposits, is a very important factor for periodontal disease progression. Inflammation of the gingiva, as an early clinical symptom of periodontitis, is considered to be a risk factor which increases susceptibility to the onset and progression of periodontal disease [16]. This is why, other than gingival curettage, the low level laser is used to prevent and attenuate the inflammatory process and facilitate recovery [17] ; [18].
Inflammation of the gingiva, as a host's response to bacterial challenge, causes detachment of the soft tissue from the teeth, making the gingival sulcus deeper, which leads to the formation of a periodontal pocket. Good oral hygiene decreases gingival inflammation and anti-inflammatory effects of therapeutic procedures make tissue regeneration possible [19]. A sub-gingival curettage technique is performed to reduce the pocket depth by decreasing the inflammatory process and thus speed up recovery.
Periodontal treatment eliminates inflammation and contributes to an improvement in the disease. In addition to conventional periodontal therapy, which includes mechanical treatment of periodontal pockets [20], antibiotic [21] and surgery [22], lasers (high level lasers in periodontal surgery and low level lasers for their biostimulating effects) are currently very successfully applied as adjunct therapeutic device in the treatment of periodontal disease [23].
The results of the examination connected to PI values showed that both groups had similar plaque values before therapy (E: 1.70 vs. C: 1.65). There was a considerable decrease of PI values three months after application of both therapies (E: 1.00 vs. C: 1.06). This decrease in the PI index is the result of patients’ education in maintaining oral hygiene, thus removing inflammatory effects of microbes and their products on gingival tissue. Application of combined therapy leads to decrease in PI within the time frame before therapy, and 3 and 6 months after therapy (E: 1.70; 1.00; 0.94). It also shows a tendency to decrease compared to conservative therapy where PI values decrease three months after the therapy, but six months after the therapy they rise again and approach the values that they had before the therapy was applied (C: 1.65; 1.06; 1.46) (Table 2). These results are in accordance with the results of Angelov's research [24].
The inhibition mechanism of dental plaque by the laser is not clear. Further experimental studies are needed to examine the effects of the laser on the metabolism of vital cells in dental plaque. This effect may help explain the laser light effect on gingival inflammation by decreasing plaque bacteria.
The results from this study showed that the mean CAL values in patients from both groups before therapy were similar (E: 1.58 mm vs. C: 1.62 mm). Three months after the application of both conservative and combined (conservative complemented with laser) therapy, there is a considerable CAL decrease in the gingival status (E: 0.94 mm vs. C: 1.08 mm) as a consequence of the therapeutic procedure. In the control period after 6 months, the CAL values continue to decrease in the experimental group (E: 0.61 mm), whereas there is only a slight decrease in the CAL values in the control group (C: 0.98 mm). The testing results of the CAL values show that there is no statistically significant difference between the two groups of patients (p = 0.699; p = 0.270) in the CAL values before the therapy, and 3 months after the therapy. However there is a statistically significant difference in the CAL values in the control after 6 months (p = 0.006).
Conclusion
Some important conclusions can be drawn from the analysis of the results obtained. Examinations have shown that the PI values decreased after laser therapy. While determining CAL and BOP values, after laser radiation a statistically significant improvement in values was observed, especially over longer periods of six months. Based on histological findings of the examined gingiva, we can say that it is justifiable to use the low level laser in the treatment of gingival inflammation.
These reported conclusions lead to the general conclusion that LLLT can be used as an adjuvant, very successful physical method of treatment, which together with conservative periodontal therapy, gives better results and has an influence on the long-term effects of the achieved therapeutic results.