Abstract: In current dental practice, restorative and endodontic procedures have been developed in an attempt to preserve the vitality of dental pulp after exposure to external stimuli such as caries infection. When damage to dental pulp is reversible, pulp wound healing can proceed, whereas irreversible damage induces pathological changes in dental pulp, eventually requiring its removal. Furthermore, dentists sometimes extract non-vital teeth because of severe caries progression, critical size of periapical lesion, and tooth fracture. To overcome the limitations of presently available therapies, it is important to develop regeneration therapy for dental pulp and periapical tissues. In this review, we focus on the regeneration of dental pulp and periapical tissues by application of exogenous growth factors and scaffolds, as well as low-intensity laser irradiation as an auxiliary therapy for regeneration therapy.
Keywords: dental pulp regeneration; regeneration of bone defects; FGF2; gelatin hydrogels; laser irradiation
1. Introduction
One of the universal facts for dentists is that preservation and maintenance of dental pulp viability are essential to avoid tooth loss. Dental pulp is sometimes affected by external stimuli such as caries infection or traumatic injury. In current dental practice, when dentists find a deep dental caries with vital and reversible dental pulp, they remove infected enamel and dentin, and carry out restorative procedures with pulp capping or pulpotomy. Pulp capping and pulpotomy with biomaterials such as calcium hydroxide are accepted as effective procedures to induce pulp wound healing, including some processes such as apoptosis of odontoblasts and dental pulp cells in the initial phase, followed by reactionary and reparative dentinogenesis in the late phase [1-5]. Reactionary dentin is formed by surviving odontoblasts, and reparative dentin is formed by odontoblast-like cells differentiated from dental pulp stem cells or residual dental pulp [6-8].
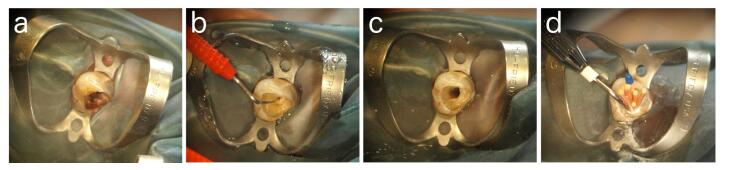
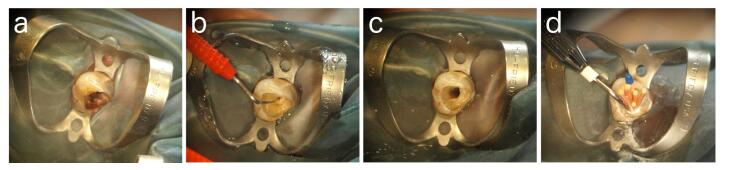
When dentists find a severe defect with a critical size of the resultant exposure of dental pulp, there are no effective treatments to preserve the viability of dental pulp from the irreversible damage, and dentists carry out endodontic procedures including complete removal of dental pulp (pulpectomy),irrigation of the root canal mechanically and chemically to regulate inflammatory responses of apical area of the periodontal ligament, and fill the root canal with biomaterials such as a gutta-percha to prevent re-infection by bacteria (Figure 1).
Figure 1. (a) Before pulpectomy of left maxillary canine; (b) Dental pulp exposure after removal of infected dentin; (c) Root canal after preparation and irrigation; (d) Root canal filling.
Furthermore,
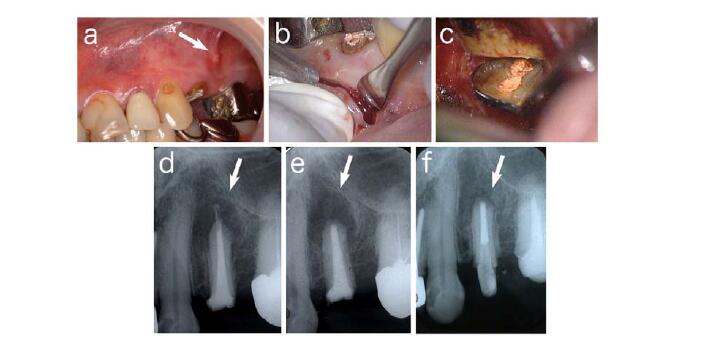
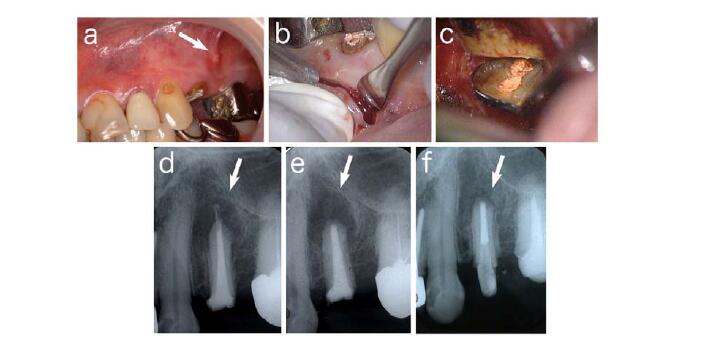
Furthermore, persistent periapical lesion at a treated tooth sometimes occurs because of its complicated anatomical structure or inadequate treatment by dentists. Dentists carry out endodontic surgery such as apicectomy to induce wound healing and regeneration of periapical tissues (Figure 2).Figure 2. (a) Fistula formed at buccal site of left maxillary first premolar; (b) Incision for apicectomy; (c) After removal of root apex and infected granulation tissue;
(d) Radiophotograph of (a). Periapical lesion (arrow) was observed; (e) After apicectomy.Bone defect (arrow) was observed; (f) Three months after surgery. Bone formation (arrow) was observed.
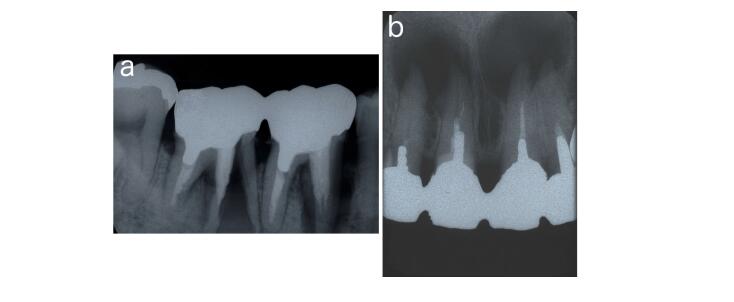
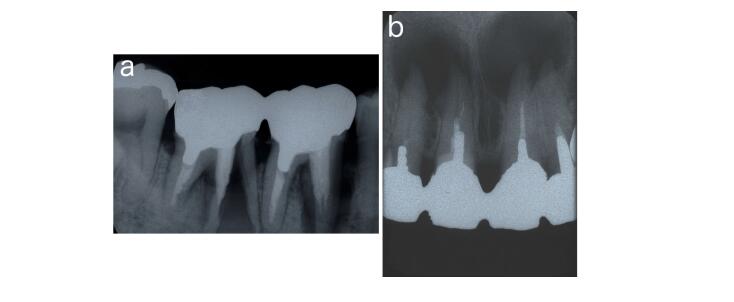
However, a tooth without vital dental pulp has lost its defensive ability, which is often followed by severe damage such as progression of deep radicular caries or tooth facture, resulting in the extraction of the tooth to preserve further expansion of the uncontrollable infection (Figure 3). It is reported that the success rate of endodontic retreatment is lower than that of initial treatment [9-12].
To overcome these limitations in the available therapy to preserve a functional tooth in the present dentistry, it is important to develop regeneration therapy for dental pulp and periapical tissues.
Figure 3. (a) Root fracture of right mandibular second molar; (b) Critical size of periapical lesion of maxillary incisors.
2. Strategies for Local Regeneration of Dental Pulp and Periapical Tissues
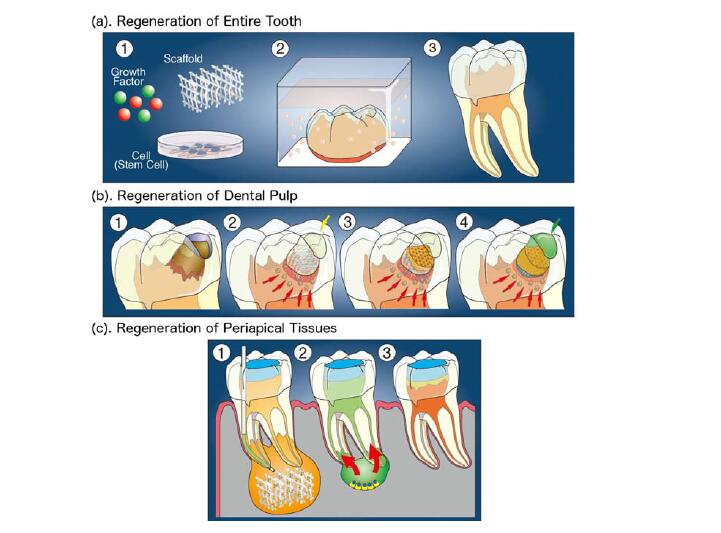
It is well known that essential three factors to achieve tissue engineering are stem cells, growth factors, and scaffolds [13]. Stem cells, which are supplied from tissues around or outside of the target area, differentiate into specific cells to regenerate tissue defects. Growth factors such as bone morphogenetic proteins (BMPs) and fibroblast growth factors (FGFs), which are mainly supplied from outside of the target, induce proliferation and differentiation of stem cells. Scaffolds with properties of extracellular matrix temporally support structures for cell growth, differentiation, and tissue formation. In research for tissue regeneration of dental pulp and periapical tissues, these three factors are appropriately combined and applied to the target area.
Figure 4. Schemes of strategies for the regeneration therapy of dental pulp and periapical tissues. (a) Regeneration of the entire tooth. In the strategy, a tooth germ is regenerated by growth factors, scaffolds, and stem cells in organ culture; (b) Regeneration of dental pulp and dentin. This strategy is further classified into two ways. One is the regeneration by the combination of supplied tissue engineering factors including growth factors, scaffolds, and stem cells. The other is the regeneration by supplied growth factors and scaffolds, and stem or progenitor cells are induced from residual tissues; (c) Regeneration of periapical tissues by the combination of tissue engineering factors with external stimulation such as laser irradiation.
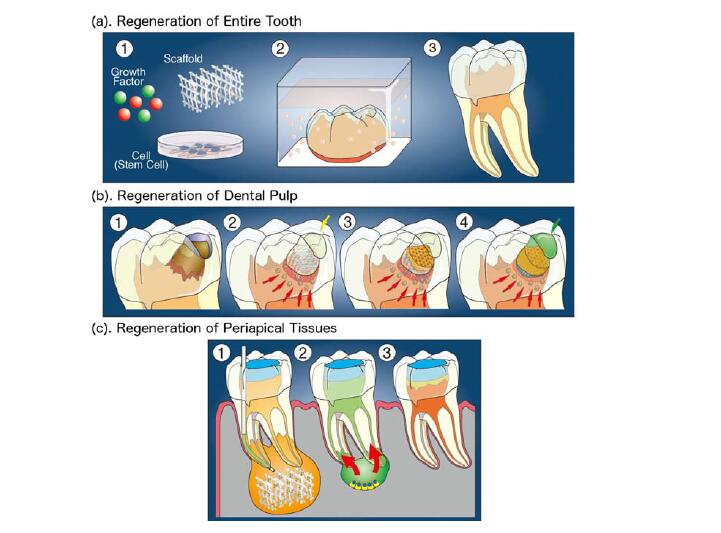
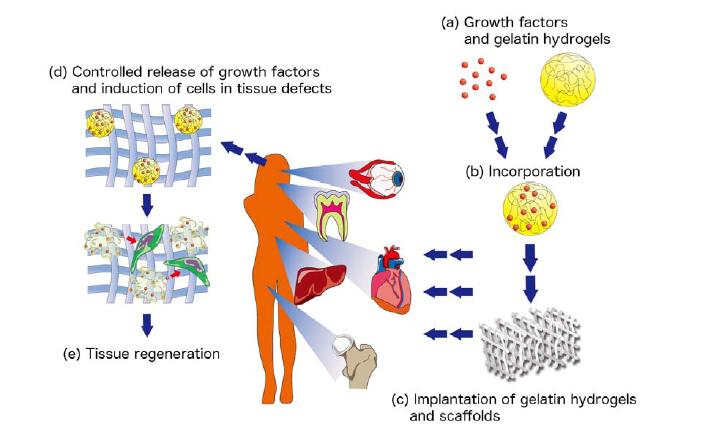
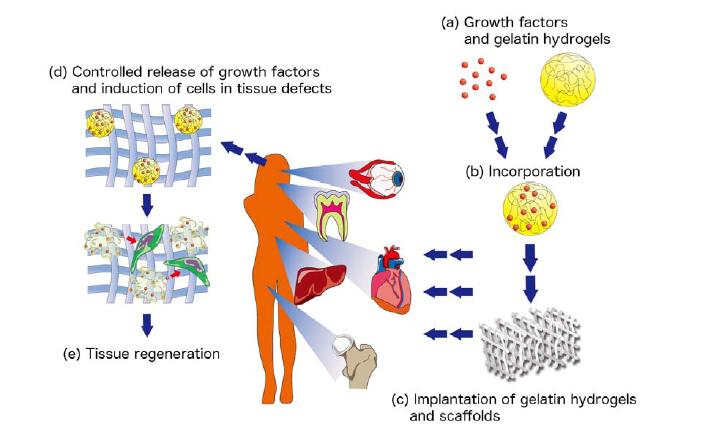
Figure 5. Scheme for controlled release of growth factors from gelatin hydrogels.(a,b) Preparation of gelatin hydrogels incorporating growth factors. Growth factors are impregnated into gelatin hydrogels through immersion of gelatin hydrogels into solution of growth factors; (c) Implantation of gelatin hydrogels incorporating growth factors with scaffolds such as collagen sponge into a tissue defect area; (d,e) In the defect area, growth factors are gradually released from gelatin hydrogels through the biodegradation of gelatin hydrogels by collagenase or gelatinase. This controlled release of growth factors induces stem or progenitor cells into the scaffold, resulting in the regeneration of tissue into target area.
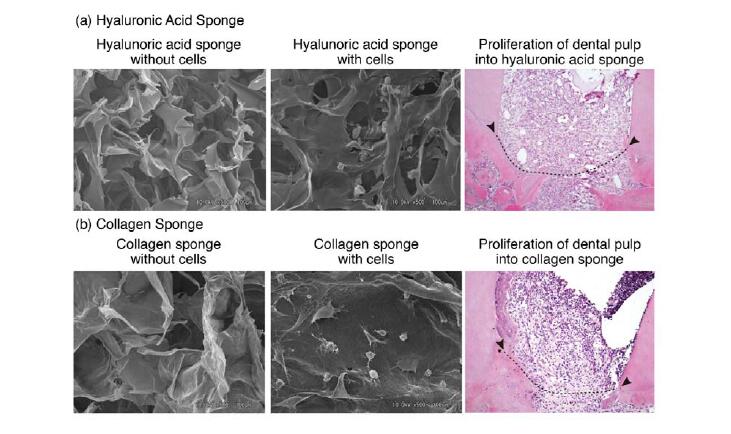
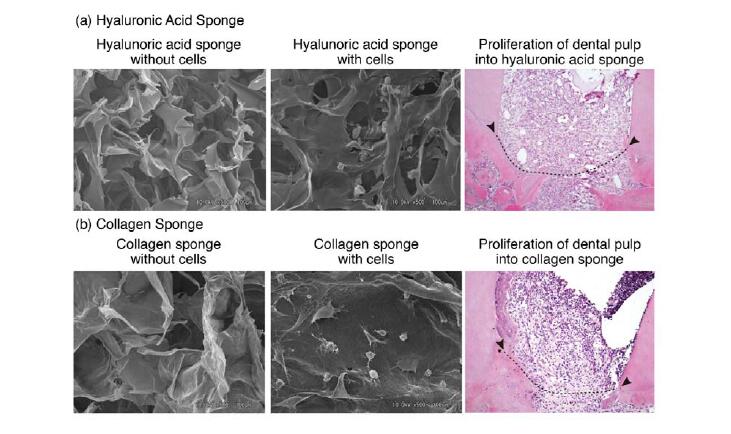
Recently, we examined the in vitro and in vivo compatibility of HA sponge for regeneration of dental pulp by comparison of HA sponge with collagen sponge. We used KN-3 cells, which were established from rat dental pulp, have odontoblastic properties such as high alkaline phosphatase activity and calcification ability [100]. In vitro results showed that KN-3 cells adhered to HA sponge,as seen in collagen sponge. In vivo results, following implantation of both sponges in dentin defect areas, showed that dental pulp proliferation and invasion of vessels into both sponges were well induced from amputated dental pulp, suggesting that HA sponge has an ability to sustain dental pulp tissue regenerated from residual
dental laser tips amputated dental pulp. Furthermore, we found that the inflammatory responses of KN-3 cells and the amputated dental pulp to HA sponge were lower than those against collagen sponge, suggesting that HA sponge has biocompatibility and biodegradation characteristics as well as an appropriate structure to make it suitable for dental pulp regeneration [101] (Figure 8).
Figure 6. (a) Effects of hyaluronic acid sponge on KN-3 cells and amputated dental pulp;(b) Effects of collagen sponge on KN-3 cells and amputated dental pulp. Arrowheads and dotted line; amputated line of dental pulp.
Conclusion
Throughout this review, we discussed local regeneration therapy of dental pulp with dentin and periapical tissues. Except for some studies, growth factors and scaffolds are exogenously supplied as biomaterials, while the sources of stem or progenitor cells are dependent on the residual tissues. For these local regeneration therapies of dental pulp and periapical tissues, controls of infection and inflammatory responses are critical points to preserve the vitality of residual tissues. To achieve complete infection control, the development of anti-microbial dental materials with an ability to seal the defect area is important. The resin bonding system with composite resin is commonly used as one of materials showing favorable adhesion to enamel and dentin, and there are some reports about anti-microbial composite resin [103-105], which may inhibit further bacterial invasion after tissue regeneration of dental pulp and periapical tissues. Regarding the control of inflammatory responses, it has been reported that the available clinical data supporting the efficacy of BMP2 in clinical trial are not all robust [82,106,107], and inflammation at the target site may be one of the inhibitors against BMP2 induced tissue regeneration. It is important to develop exogenous supplementation of anti-inflammatory molecules, as well as an accurate method for assessing the vitality of the residual dental pulp.
Acknowledgements
This review was supported by Grants in Aid for Scientific Research (C.K., T.N., E.J.) from The Ministry of Education, Science, and Culture of Japan, Tokyo, Japan.