This article reviews the current and potential appli-cations of laser technology in nonsurgical therapy for the treatment of periodontal diseases. Based on its various characteristics, such as ablation or vaporiza- tion, hemostasis, and sterilization effect, laser treat- ment may serve as an adjunct or alternative to conventional, mechanical periodontal therapy. TheCarbon dioxide (CO2) and the Neodymium-doped:Yttrium-Aluminum-Garnet (Nd:YAG) lasers were previously approved for soft tissue treatment in periodontics (1, 2, 4), because of their superior ability of soft tissue ablation, accompanied by strong he-mostatic and bactericidal effects (6, 37, 143, 170, 218).However, when these lasers are applied to dental hard tissues the result is major thermal damage,especially at a high-energy output, rendering them unsuitable for hard tissue treatment (56, 214).Recently, the Erbium-doped:Yttrium-Aluminum-Garnet (Er:YAG) laser was developed in dentistry (71,85, 87). As it is capable of ablation in both soft and hard tissues, the Er:YAG laser can be used for perio-dontal hard tissue treatment such as root surface debridement, as well as soft tissue management (78).The use of lasers within the periodontal pocket has become a topic of much interest and is a promising field in periodontal therapy. This article deals with recent advances in nonsurgical laser therapy for periodontal disease, and will briefly describe the advantages and disadvantages of various laser types.
Nonsurgical periodontal therapy and lasers In periodontal pockets, the root surfaces are con- taminated with an accumulation of plaque and cal- culus, as well as infiltration of bacteria and bacterial endotoxins into cementum (5). Complete removal of these harmful substances is essential for the healing of periodontal tissue. Formation of biofilms on the exposed root surface within periodontal pockets impedes the infiltration of antibiotics, and therefore mechanical disruption of the biofilm is necessary during periodontal treatment (36).
Basically, the aim of periodontal treatment is to restore the biological compatibility of periodontally diseased root surfaces for subsequent attachment of periodontal tissues to the treated root surface. During the initial periodontal treatment, debridement of the diseased root surface is usually performed by mechanical scaling and root planing using manual or power-driven instruments. Power-driven instruments (power scalers) such as ultrasonic or air scalers are frequently used for root surface treatment as they render the procedure easy and less stressful for the operator, while improving the efficiency of treatment. However, conventional mechanical debridement using curettes is still technically demanding and time consuming, and power scalers cause uncomfortable stress to the patients from noise and vibration.Complete removal of bacterial deposits and theirtoxins from the root surface and within the perio-dontal pockets is not necessarily achieved with con-ventional, mechanical therapy (5). In addition, access to areas such as furcations, concavities, grooves, and distal sites of molars is limited. Although systemic and local antibiotics are occasionally administered into periodontal pockets for the purpose of disinfec-tion, with frequent use of antibiotics there is a potential risk of producing resistant microorganisms.Therefore, development of novel systems for scaling and root planing, as well as further improvement of currently used mechanical instruments, is required.
As lasers can achieve excellent tissue ablation with strong bactericidal and detoxification effects, they are one of the most promising new technical modalities for nonsurgical periodontal treatment. Another advantage of lasers is that they can reach sites that conventional mechanical instrumentation cannot.The adjunctive or alternative use of lasers withconventional tools may facilitate treatment, and has the potential to improve healing.
Conventional mechanical treatment usually pro-duces a smear layer and, sometimes, deep grooves on the root surface. A smear layer may adversely affect the healing of periodontal tissues as it contains bacteria and inflammatory substances such as debris of infec-ted cementum and calculus (140). Therefore, ways to eliminate the smear layer have been investigated in recent years. Many researchers have examined the effects of root conditioning after mechanical debri- dement, using chemical agents such as tetracycline, citric acid, and ethylenediaminetetraacetic acid (EDTA). Root conditioning has been shown to remove the smear layer, and to expose collagen fibers and dentinal tubules, enhancing the histocompatibility and new connective tissue attachment with cement- ogenesis (25, 120, 154). Laser irradiation has been reported to exhibit bactericidal and detoxification ef- ects without producing a smear layer, and the laser- treated root surface may therefore provide favorable conditions for the attachment of periodontal tissue.
Gingival curettage after scaling and root planing using mechanical instruments has been shown to have no added benefit over routine scaling and rootplaning (3, 41, 108, 146). Therefore, the root surface has been the focus of mechanical debridement, and root surface debridement alone is the main step of nonsurgical periodontal therapy at present. However, the poor clinical outcome of gingival curettage may have been due to the lack of an effective tool for soft tissue debridement. Contrary to mechanical treat- ment with conventional instruments, the excellent ablation of tissue with laser treatment is expected to promote healing of periodontal tissues, ablating the inflamed lesions and epithelial lining of the soft tissue wall within periodontal pockets. This procedure might be more effective for the treatment of residual pockets after initial therapy and during maintenance.
Part of the laser energy scatters and penetrates during irradiation into periodontal pockets. The attenuated laser at a low energy level might then sti-mulate the cells of surrounding tissue, resulting in reduction of the inflammatory conditions (131, 162,183), in cell proliferation (8, 103, 135), and in increased flow of lymph (184), improving the periodontal tissue attachment and possibly reducing postoperative pain.
Although there is no clear evidence to date that laser applications improve clinical outcome due to the action of curettage (3), laser treatment has a potential advantage of accomplishing soft tissue wall treatment effectively along with root surface debridement, and should be further investigated. Characteristics of laser ‘LASER’ is an acronym for Light Amplification by Stimulated Emission of Radiation. The physical principle of laser was developed from Einstein’s theories in the early 1900s, and the first device was introduced in 1960 by Maiman (114). Since then, lasers have been used in many different areas in medicine and surgery. Laser light is a man-made single photon wavelength. The process of lasing occurs when an excited atom is stimulated to emit a photon before the process occurs spontaneously. Spontaneous emission of a photon by one atom stimulates the release of a subsequent photon and so on. This stimulated emission generates a very coherent (synchronous waves), monochromatic (a single wavelength), and collimated form (parallel rays) of light that is found nowhere else in nature(28). Lasers can concentrate light energy and exert a strong effect, targeting tissue at an energy level that is much lower than that of natural light. The photon emitted has a specific wavelength that depends on the state of the electron’s energy when the photon is released. Two identical atoms with electrons in identical states will release photons with identical wavelengths. The characteristics of a laser depend on its wavelength(Table 1, Fig. 1).
The term ‘waveform’ describes the manner in which laser power is delivered over time, either as a con-tinuous or as a pulsed beam emission. A continuous wave laser beam emits an uninterrupted beam at the output power set for as long as the switch is turned on. The pulsed beam may be delivered in two different modes: free-running pulse, in which pulsation occurs within the laser tube, and gated (chopped) pulse, in which the continuous wave beam is interrupted by a shutter at various rates. The gated pulse has the same maximum power as that set on the control panel of the laser, whereas the free-running pulse is the result of power storage for given time periods. Release of stored power within a very short time creates an emissionthat exhibits a peak power greater than the power selected on the control panel (28, 159).
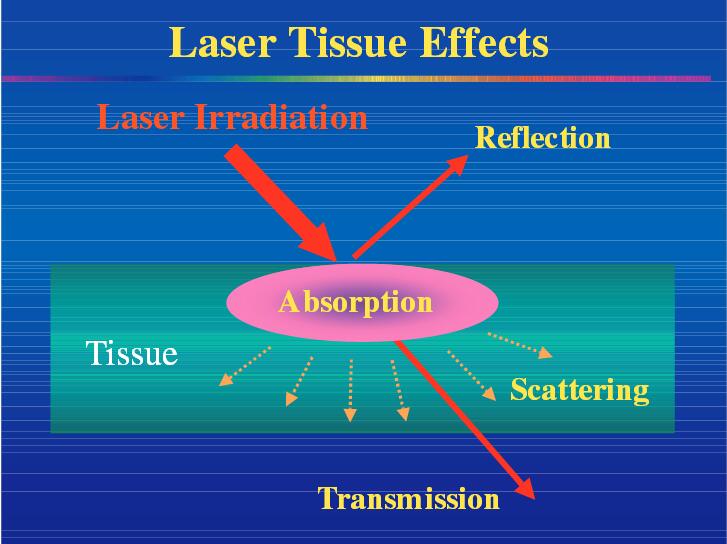
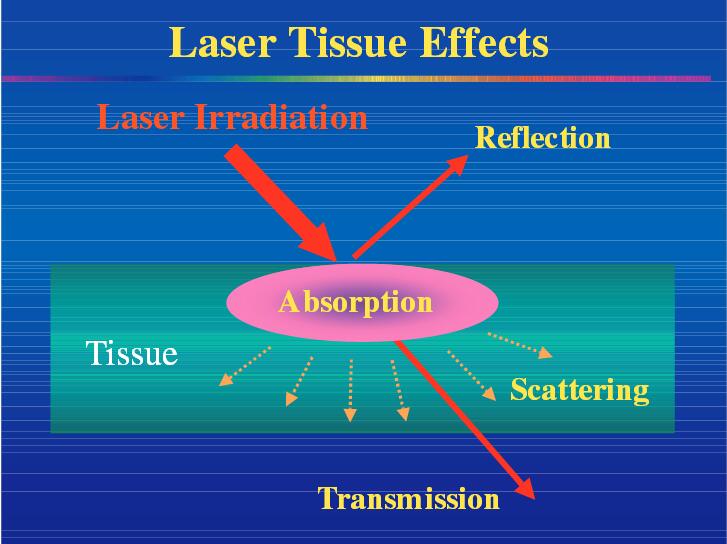
When laser light reaches a tissue, it can reflect,scatter, be absorbed or be transmitted to the sur-rounding tissues (Fig. 2). In biological tissue, absorption is mainly due to the presence of free water molecules, proteins, pigments, and other macromolecules. The absorption coefficient strongly depends on the wavelength of the incoming laser irradiation.