A desktop diode pulsed laser having pulse width of 1.3 ps and wavelength of 1552 nm is utilized for pre- cise targeted ablation of dentin, enamel, and composite material while minimizing thermal damage to the surrounding healthy tissue and nerve endings. A thermal imaging camera is used to measure the den- tal surface temperature rise during ablation. Following ablation, scanning electron microscopy (SEM) and optical microscopy are used to determine the quality of ablation and the volumetric ablation rate as a function of laser parameters. Surface temperature measurements are compared with the numerical mod- eling results obtained using the transient heat conduction equation. A good agreement between experi- mental and modeling results for the surface temperature is obtained which ensures accurate prediction of the temperature distribution throughout the tooth using numerical models. The SEM generates images of precise ablation of each dental material when the optimal laser parameters are used and the sample is scanned at a velocity to limit the number of overlapping pulses. During the ablation process there is min- imal collateral damage to the surrounding healthy tissue and minimal heat spread throughout the tooth thus preserving the integrity of the pulp.
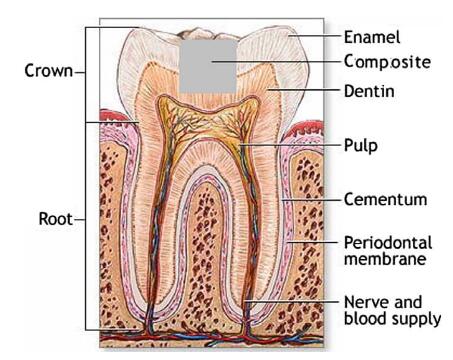
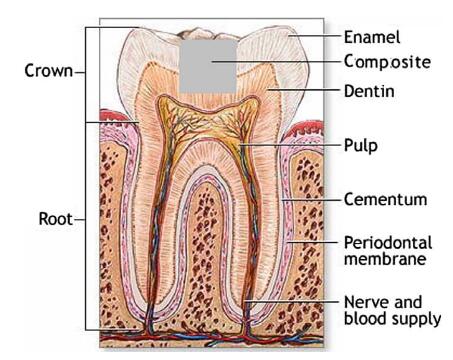
1. Introduction Lasers have been of interest to the medical community for many years and have become a common instrument for many current medical procedures. For more than 40 years, lasers have been investigated for dental applications [1]. Currently, lasers in den- tistry are primarily used for the ablation, or removal, of soft human tissue for periodontal disease and cosmetic surgery [2,3]. However, over this time, lasers have yet to become a common device used in dental offices for the ablation of hard tissue (enamel and dentin), caries, and filling material (composite and amalgam) for cavity preparation due to low ablation rates and thermal dam- age produced by many of the lasers studied over the last four dec- ades. Caries removal and the preparation of cavities in dentistry are still primarily performed by the use of mechanical drills. These drills are often limited in precision resulting in a large amount of healthy enamel and dentin to be lost while removing the decayed tooth. This current technique is invasive and causes patient dis- comfort. The discomfort associated with mechanical drilling can be a psychological barrier for patients to overcome in seeking proper dental care. Due to the vibrations of the drills, it is necessary to use local anesthetic for the majority of dental procedures. A con- tinuous water spray is used in conjunction with the drills to bal- ance the temperature rise produced by friction between the drill and the tooth. Most tooth decay occurs in the enamel (outer sur- face) and the dentin, which is the region between the enamel and inner region of the tooth containing the nerve endings (pulp).
In order to utilize lasers for caries therapy (removal of tooth de- cay), it is crucial to minimize the amount of heat diffusion to the surrounding tooth due to thermal energy produced by the laser irradiation. The human tooth is extremely sensitive to temperature variation such that a patient can sense a change in local tempera- ture at the pulp of ±4 ° C [5]. To protect the nerves contained in the pulp of the tooth from irreversible damage, such as permanent nerve loss, the temperature rise cannot exceed 10 ° C [6–8] . Studies performed by Zach and Cohen [9] have shown that temperature rise of 20 ° C in the pulp of the tooth almost always caused irrevers- ible nerve damage. For temperature rises in the pulp of 10 ° C there is a 15% chance that irreversible nerve damage will occur [9]. The pulp is extremely sensitive to temperature variations because of the nerve endings and blood flow contained within the pulp cham- ber. Alternatively, dental enamel and dentin can withstand higher temperature levels as long as thermal or mechanical damage (melting or cracking) is not induced. Prior research on the ablation of human hard tissue has been primarily performed using a variety of long-pulsed lasers over a range of wavelengths. Recent investigation by some researchers has demonstrated precise selective ablation of composite restorations and fissure sealants [10] using a frequency-tripled Nd:YAG laser. Though long-pulsed lasers have been used to ablate dental hard tissue efficiently, they produce a large amount of ther- mal diffusion throughout the tooth causing thermal/mechanical damage to the tooth structure as well as physical damage to the nerves [8]. It has been determined that direct ablation using long-pulsed lasers with pulse durations larger than 10 ps will in- crease the heat-affected zone, resulting in a thermal ablation in dielectrics such as teeth [11–15] . Thermal ablation occurs when a material absorbs enough radiant energy from the laser pulses to heat it to the boiling point temperature – at this temperature the material becomes vaporized [16]. According to Niemz [7], long- pulsed lasers and continuous-wave lasers generate a substantial amount of heat in hard tissue such as human teeth because the pulse duration is too long, allowing heat to diffuse significantly throughout the tooth and ultimately rising the pulp temperature far above the 10 ° C temperature rise threshold for irreversible nerve damage.
Numerical analysis of heat diffusion in the tooth caused due to laser irradiation during dental ablation is extremely important to validate the safety of dental procedures for future clinical investi- gations. Knowledge of the temperature rise at the pulp chamber is crucial in order to guarantee that the nerves will not become per- manently damaged from the heat. Experimental measurement of the temperature rise within the pulp of the tooth is very difficult to achieve. The structure of the human tooth is hard and brittle, which makes if very difficult to drill small holes to insert thermo- couples, without causing a large amount of tooth loss. Even if a few holes are created to insert thermocouples a small number of points will be measured and the thermocouples can give false tempera- ture measurements due to the absorption of light by the thermo- couples [25]. The best way to determine the temperature rise at the pulp of the tooth for a variety of laser parameters and many points throughout the tooth is to use the heat conduction model to predict the temperature rise in the pulp chamber.
2. Experimental methods and materials A schematic of the experimental setup is shown in Fig. 1 . The laser used in this study is a desktop ultra-short-pulse fiber laser (Raydiance Inc.) operating in the near-IR region having a wave- length of 1552 nm and pulse duration of approximately 1.3 ps. The laser beam is focused on extracted human teeth samples using a20 microscope objective with a working distance of approxi- mately 21 mm to produce a focal spot size diameter of roughly 10 l m. The array of time-averaged power values that can be pro- duced by the laser varies from 0.040 W to 2.50 W through the adjustment of both the energy per pulse which varies from 1 l J/ pulse to 5 l J/pulse and the repetition frequency which varies be- tween 25 kHz and 500 kHz. Extracted human teeth samples were obtained from Bright Now Dental in Satellite Beach, FL. Teeth samples included 10 healthy teeth and 10 teeth containing fillings (composite material). The composite material (Prime and Bond NT, DENTSPLY Caulk, Milford, DE) is a light-cured dental adhesive system that combines compos- ite materials to the dentin and enamel of the tooth for direct com- posite cavity restoration. The composition of Prime and Bond NT includes dimethacrylate and trimethacrylate resins, PENTA (dip- entaerythritol penta acrylate monophosphate), nanofillers- amor- phous silicon dioxide, photoinitiators, stabilizers, cetylamine hydrofluoride, and acetone.
The extracted teeth were machined first with a dental drill and then with a surface grinder so that the crown of the tooth was re- moved resulting in a flat surface exposing dentin, enamel, and composite filling on which the laser beam is easily focused. The la- ser beam is focused directly on the surface of the machined tooth where the ablation is desired. The sample was positioned on a three-axis stage driven by high-speed Newport SMC 100 motion controllers interfaced with National Instruments Lab view 8.0 to run the controllers. The maximum velocity of these controllers is 25 mm/s and can be varied in steps of 50 l m/s. A detailed parametric study is performed to determine the abla- tion quality, surface radial temperature rise, and volumetric abla- tion rate as a function of laser parameters such as time-average power, repetition rate, and energy per pulse. During ablation, an infrared camera (IR Flexcam Pro, Infrared Solutions, Victoria, AU) is used to monitor the tooth’s surface temperature. Thermal cam- era data is processed to generate radial surface temperature rise plots which will be compared to the calculated values for the sur- face temperature rise using the transient heat conduction equa- tion. Following the dental ablation experiments, a scanning electron microscope (JEOL JSM 6380LV, Tokyo, Japan) is used to determine the quality, precision and width of the ablation trench created in each material (enamel, dentin and composite filling). An optical microscope on a Scanning Probe Microscope (PSIA, XE- 100, Santa Clara, CA) is used to measure the ablation depth in the dental materials with an accuracy of 0.1 l m.