Conventional dentistry involves using rigid metal or diamond instruments to drill, cut, or abrade hard and soft tissues. Traditional dental treatment is recognized as the process of removing infected or pathologic tissue by either drilling or cutting away the diseased component.2 Dental lasers can be used to cut, incise, and ablate hard and soft tissues. The inherent properties of laser light—such as selective absorption, coagulation, sterilization, and stimulatory effects on vital structures—make lasers the treatment of choice in certain clinical scenarios.
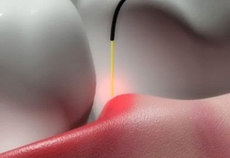
Proper clinical technique is extremely important when lasing a patient’s oral tissues. It is strongly recommended that the operator use proper magnification and illumination to assess the treatment’s progress accurately and determine that photothermal ablation is occurring. A definitive color change will be observed at the initial moment of tissue ablation; at that point, the clinician should move the laser tip in a slow and deliberate “paint brushing” motion that corresponds to the patient’s specific tissues, always evaluating the laser/tissue interaction to obtain the optimal result. Many new laser users make the common error of using a fast and constant painting motion and moving the beam too quickly; this improper technique will not allow proper ablation to occur. Electrosurgery, or electrocautery, is not absorption-specific within a target tissue; as a result, extremely high temperatures are created within the tissue mass to produce a desired clinical effect known as fulguration. Electrosurgical techniques used at present for tissue ablation are unable to control the depth of necrosis in the tissue being treated. Most electrosurgical devices rely on the creation of an electric arc (between the treating electrode and the tissue that is being cut or ablated) to cause the desired localized heating. These high temperatures cause a depth of necrosis of more than 500 μm (often more than 800 μm and sometimes as high as 1,700 μm); the inability to control such depth of necrosis is a significant disadvantage to using electrosurgical techniques for tissue ablation.8 Lasers do not suffer from electrical shorting in conductive environments and certain types of lasers allow for very controlled cutting with limited depth of necrosis, due to their inherent ability to absorb chromophores within a specific target tissue.For the purpose of this article, clinical applications for lasers in dentistry are separated into three different groups: soft tissue treatment, hard tissue treatment, and non-surgical treatment.
Soft tissue lasers
Overall, dental lasers are relatively easy to use, as long as the clinician has been trained properly. It is important to understand that lasers function with an “end cutting” action (that is, laser energy is emitted from the end of the laser), while most other dental instruments are “side cutting,” with the cutting edges or abrasive surfaces located on the lateral surface. Although most laser soft tissue treatments heal by secondary intention, the postoperative course usually is uneventful.9 Most laser excisional or incisional procedures are accomplished at 100°C, where vaporization of intra- and extracellular water causes ablation or removes biological tissue. Clinicians must be wary of the heat generated within tissues during a procedure. If the tissue temperature exceeds 200°C during a lasing procedure, carbonization and irreversible tissue necrosis will occur.6 This adverse consequence can be avoided completely by using the lowest power setting necessary to achieve the desired treatment goal. There are specific soft tissue indications for the clinical use of lasers, including anterior gingival esthetic recontouring, gingivectomy/gingivoplasty (for crown lengthening procedures), operculectomy, removal of epuli, incisions when laying a flap, incision and drainage procedures, frenectomy, vestibuloplasty, coagulation of extraction sites, treatment of herpetic and recurrent aphthous ulcer lesions, uncovering of an implant, pre-impression sulcular retraction, and ablation of an intraosseous dental pathology (such as a granuloma or an abscess). Other excisional laser procedures involve the removal of soft tissue targets that may appear as benign lesions (such as fibromas or papillomas) on the lip, tongue, buccal mucosa, or palatal area; the removal of coronal pulp as an adjunct to root canal therapy; excisional biopsy; and sulcular debridement.
Diode (810 nm, 940 nm, 980 nm, 1,064 nm)(Pioon laser systems provide), Nd:YAG (1,064 nm), CO2 (10,600 nm), Er:YAG (2,940 nm), Er,Cr:YSGG (2,780 nm), and potassium-titanyl-phosphate (KTP) (532 nm) lasers are the wavelengths used most commonly for soft tissue procedures.2 Diode and Nd:YAG lasers are alike in that these lasers are absorbed in pigmented tissues (melanin and Hb) and both wavelengths are transmitted to their targets in contact with a thin flexible quartz fiber. CO2 laser energy is absorbed in the target tissue’s water content and transmitted to the intended target using a hollow waveguide or an articulated arm. Erbium laser energy is transmitted to the intended target tissue by a clear sapphire or quartz tip, either in contact or approximately 0.5 mm from the target.2 Each wavelength has its own unique interactive qualities and a different clinical feel that operators must experience to attain a certain comfort level. A soft tissue crown lengthening procedure can be accomplished by using any of the laser wavelengths mentioned above.