

When sensitivity occurs during ultrasonic debridement, clinicians should assess the ultrasonic instrument's level of energy output. This refers to the relationship between frequency, power, and other factors affecting the debridement procedure. Ultrasonic frequency impacts the speed of the ultrasonic insert/tip's (UIT) movement, while power controls the distance the UIT travels across the tooth in one vibration. Many clinicians can adjust their instruments' power output, but not their frequency because auto-tuned units do not have this capability.
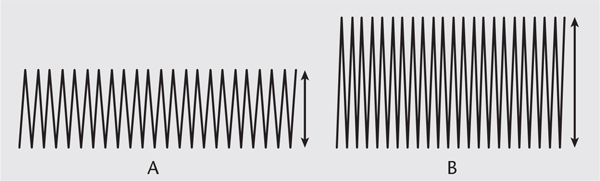 FIGURE 1. This diagram depicts amplitude or power with an ultrasonic instrument. A represents a low setting, while B designates a high setting.
FIGURE 1. This diagram depicts amplitude or power with an ultrasonic instrument. A represents a low setting, while B designates a high setting. Assessing the ultrasonic instrument's power level is critical to reducing discomfort. Adjusting the power level changes the energy output needed to remove calculus, fine deposit, and plaque biofilm. As early as 1986, researchers concluded that as amplitude increases, the output of power also grows, enhancing the chipping action of the UIT.7 Thus, an increase in power causes the UIT to travel more during a single vibration (Figure 1). Displacement amplitude varies between each UIT.7 An in vitro study evaluating tooth substance loss found a significant difference based on power setting in a magnetostrictive unit.8 The least amount of calcium was lost from the dentin when the power setting was at the lowest level.8 The loss of dentin may lead to hypersensitivity by exposing dentinal tubules to stimuli. Therefore, in susceptible patients, a low power setting may be indicated to enhance comfort. However, clinicians need to be aware of the increased risk of burnishing tenacious calculus deposits when ultrasonic instruments are used at low power.9
Regarding the duration of exposure, the longer the time spent instrumenting one area, the greater the energy delivered to the surface, which increases the likelihood of patient discomfort. To reduce this risk, clinicians should keep the UIT moving in a patterned sequence for effective debridement.10,11
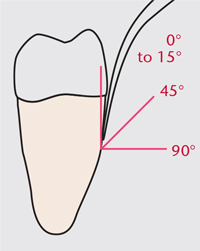 FIGURE 2. For angulation of the ultrasonic insert/tip-to-tooth, 0° to 15° is ideal for many situations.
FIGURE 2. For angulation of the ultrasonic insert/tip-to-tooth, 0° to 15° is ideal for many situations. Only the pressure needed should be applied during ultrasonic instrumentation. In most instances, the pressure, or load, is light. Significantly increasing pressure with the grasp and UIT contact could heighten sensitivity. The best approach is to let the instrument do the work. Increasing pressure might, at first, bolster the effects of the vibrating UIT; however, too much pressure can cause the energy to dampen or stop. Thin UITs are particularly susceptible to loading, which could negatively impact outcomes12 by leading to incomplete deposit removal and/or burnishing of calculus deposits.
Clinicians must also remain aware of the UIT-to-tooth angle. The greater the angle of application—up to 90°—the greater the energy output.13 The ideal UIT-to-tooth angle is 15° or less to the surface being treated (Figure 2). Significantly increasing this angle to 70° to 90° occurs most often when moving from one surface of the tooth to another such as the buccal to the mesial. Therefore, self-assessment of technique, especially at line angles, is paramount.
Additionally, the surface of the UIT being used for debridement should be evaluated. Piezoelectric tips emit the greatest energy from the back and front, while the side surfaces emit the least amount of energy. In comparison, magnetostrictive inserts emit energy from all surfaces. The point of the magnetostrictive insert emits the greatest amount of energy, while the lateral surfaces generate the least (Figure 3). Using the point of any UIT is indicated only for fracturing large, tenacious deposits. It is contraindicated on dentin and enamel because of the potential for causing defects and striations.
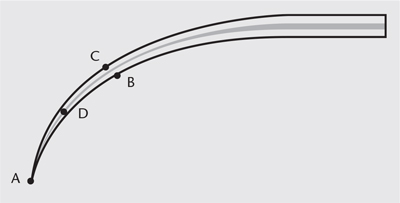 FIGURE 3. This image of a magnetostrictive insert illustrates the surfaces of its working end and the power generated at each point. A (point) generates the greatest amount of energy, B (concave) creates the second greatest amount of energy, C (convex) generates less energy than the point on concave surfaces, and D (lateral) creates the least amount of energy.
FIGURE 3. This image of a magnetostrictive insert illustrates the surfaces of its working end and the power generated at each point. A (point) generates the greatest amount of energy, B (concave) creates the second greatest amount of energy, C (convex) generates less energy than the point on concave surfaces, and D (lateral) creates the least amount of energy. Janalik et al14 noted that evaluating mechanical damage of the enamel surface during ultrasonic instrumentation is important because they found that using the point of the UIT damaged the dental enamel. There was a high variance in defect depth depending on the length of debridement and the part of the UIT that was adapted. The side of the UIT produced the shallowest defects in the shortest time period.14 In fact, using the point resulted in four times higher median values of defect depth than did using the side of the UIT in the same time period. Therefore, the authors concluded that following safety precautions when using a power-driven instrument is critical during routine debridement, and that using the side of the tip and constant movement are essential to reducing the risk of enamel damage.14 However, this study was conducted on aged canine dental enamel, which limits the veracity of the results.
Both water flow and temperature impact patient comfort. Simply stated, the greater the water flow, the lower the water temperature is in a magnetostrictive unit. Conversely, a reduced water flow leads to higher water temperatures. As such, increasing the water flow to obtain a warmer temperature might impact a patient's ability to tolerate ultrasonic instrumentation. Piezoelectric technology is immune from this issue because water is not used as a coolant for the transducer.
The effect of UIT design on sensitivity and discomfort is unclear. If sensitivity is encountered with a large, traditional UIT, trying a thin, probe-like UIT may be helpful. In a small sample of 20 patients, researchers found that a slim piezoelectric tip used for supragingival calculus removal resulted in reduced pain sensations when compared to a traditional style utilized with the same generator.15 The study also found that while debridement took longer with a slim tip when compared with a traditional tip, participants were more comfortable.15 The authors suggest this minimum amount of discomfort might enhance patient compliance with power-driven instruments.
If a tenacious deposit is challenging to remove with low power and light, overlapping strokes, clinicians should consider moving to a more productive surface of the UIT (Figure 3). If this strategy is not successful, the frequency on a manually tuned unit can be increased. Clinicians using auto-tuned units should try exerting more pressure and/or increasing the power. Moving from a fine UIT to a larger UIT may also be helpful.
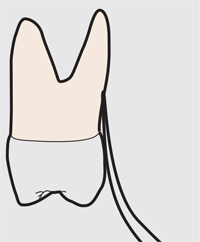
Generally, the instrument-to-tooth angle should be maintained at approximately 15° or less, with about 2 mm of the UIT's surface contacting the tooth. With biofilm removal, however, using the maximum surface area (2 mm to 4 mm) and the appropriate side of the tip is most effective, provided the adaptation fits the tooth anatomy (Figure 4). An in vitro study comparing magnetostrictive and piezoelectric devices with the same UIT design, consistent pressure, and medium power showed that the most efficient biofilm removal occurred with a side application (the convex front part) of the magnetostrictive insert.16 Both devices and UITs, however, detached biofilm when compared with the study control.16 There is potential for hypersensitivity during debridement of plaque biofilm because the UIT is in direct contact with the tooth at all times.
Many options for pain control exist in dentistry. Testing these techniques—both pre- and post-ultrasonic treatment—aids in patient comfort and acceptance. Most patients undergoing initial periodontal therapy will need local anesthesia. Even so, careful attention to correct technique is important because many of the same sensitivity triggers that occur during instrumentation may also cause permanent or temporary root sensitivity after debridement. If an endoscope is available, direct observation can be used to evaluate when complete calculus and biofilm removal is achieved and another area should be addressed. If post-operative sensitivity occurs, it might affect patient compliance with self-care and recare intervals for periodontal maintenance therapy.
Patients receiving prophylaxis may experience sensitivity during the ultrasonic procedure. These patients are often not anesthetized and may already have dentinal hypersensitivity. In this situation, an appropriate desensitizing agent should be applied prior to ultrasonic instrumentation to reduce sensation during debridement.
Striving to find the balance between relative comfort and efficacious deposit removal can be challenging. Understanding the subtle differences in energy output and remaining willing to adjust this energy can enhance patient comfort and instrument efficiency. Both the time the root is exposed to the ultrasonic energy and the contact pressure affect patient comfort. Also, how the clinician angulates the UIT and the surface of the UIT being applied are important factors to review to decrease iatrogenic patient hypersensitivity. Additionally, a low water temperature and slim tip could decrease the chances of discomfort during care. To provide safe, efficacious, comfortable, and patient-centered care, clinicians need to pay close attention to ultrasonic instrumentation technique.